Peripheral Arterial disease (PAD) is a problem with poor blood flow. It affects blood vessels outside of the heart and brain and gets worse over time. Parts of the body, like the brain, heart, arms, or legs, may not get enough blood. The legs and feet are most commonly affected. Other blood vessel problems like deep vein thrombosis (DVT), varicose veins, and chronic venous insufficiency are linked to PAD. Peripheral arterial disease (PAD) is characterized by narrowing and, in final stages, occlusion of the peripheral arteries due to atherosclerotic plaques. Smoking is the most important risk factor for developing PAD.

Epidemiology
Peripheral arterial disease (PAD) affects approximately 30% of older individuals in the general population. The principal symptom, intermittent claudication, occurs only rarely in those under 50 years of age, but increases dramatically in older individuals.
Risk factors
Modifiable risk factors
- Smoking
- Diabetes mellitus
- Arterial hypertension
- Dyslipidemia
- Homocystinuria
- Obesity
- High fibrinogen levels
- Hyperphosphatemia
- Stress
- Increased alcohol consumption
Nonmodifiable risk factors
- Family history: cardiovascular events in first-degree relatives below the age of 55 (♂)/65 (♀)
- Age: males ≥ 45 years, females ≥ 55 years (postmenopause)
Etiology
- Insufficient tissue perfusion due to atherosclerosis in the aorta and peripheral arteries. Atherosclerotic plaques reduce the arterial lumen → arterial insufficiency distal to the occlusion.
- Diabetes, the high blood sugar level present with diabetes can, over time, damage blood vessels. This makes them more likely to become narrow or to weaken.
- Arteritis can cause narrowing or weakening of the arteries. Some autoimmune conditions lead to vasculitis.
- The inflammation and scarring caused by infection can block, narrow, or weaken blood vessels. Both salmonellosis (infection with Salmonella bacteria) and syphilis are two infections traditionally known to infect and damage blood vessels.
- Defects in the structure of a blood vessel can cause narrowing. Most of these are acquired at birth, and the cause is unknown. Takayasu disease is a vascular disease that damages the aorta, the large blood vessel carrying blood from the heart to the body. It is most common among females of Asian origin.
- Blood vessels can be injured in an accident such as a car wreck or a bad fall.
Fontine Classification
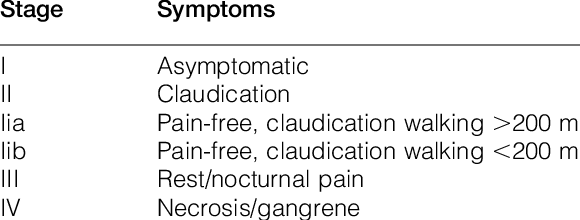
Clinical Features
- Changes in the skin, including decreased skin temperature, or thin, brittle, shiny skin on the legs and feet.
- Weak pulses in the legs and the feet
- Gangrene (dead tissue due to lack of blood flow)
- Hair loss on the legs
- Impotence
- Wounds that won’t heal over pressure points, such as heels or ankles
- Numbness, weakness, or heaviness in muscles
- Pain (described as burning or aching) at rest, commonly in the toes and at night while lying flat
- Paleness when the legs are elevated
- Reddish-blue discoloration of the extremities
- Restricted mobility
- Severe pain when the artery is very narrow or blocked
- Thickened, opaque toenails

Complications
- Arterial ulcer – Punched-out ulcer with well-defined borders. Usually involves the foot, particularly pressure points (e.g., lateral malleolus, tips of the toes).Often severe pain.
- Infection of ulcers; sepsis
- Acute limb ischemia
- Complications of endovascular intervention
- Surgical complications: bleeding, infection of vascular prosthesis, relapse.
Diagnosis
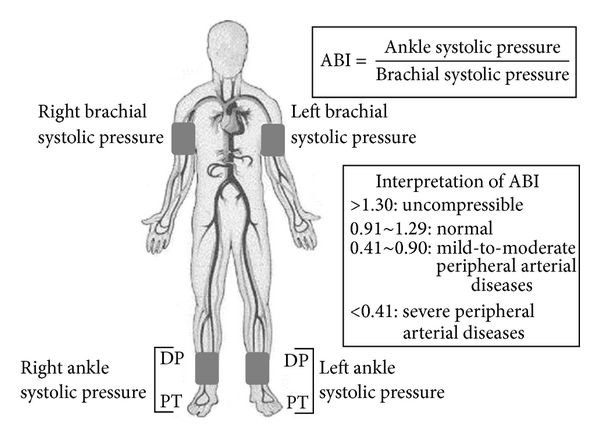
Ankle-brachial index (ABI)
- First-line diagnostic test (high specificity and sensitivity)
- Defined as the ratio of systolic ankle blood pressure (BP) to systolic brachial BP
- The ABI is calculated for each leg by dividing the higher systolic pressure of either the dorsalis pedis or posterior tibialis of the respective leg by the higher blood pressure of either the right or left arm.
- Right ABI = highest systolic BP in the right ankle/brachial BP in the arm with the highest systolic pressure
- Left ABI = highest systolic BP in the left ankle/brachial BP in the arm with the highest systolic pressure
- Normally, ankle BP and brachial BP are equal (ABI = 1), or ankle BP is only slightly higher because of gravity (ABI > 1)
- Differences in systolic BP indicate different pathologies:
- > 1.3 = medial sclerosis with incompressible vascular wall (generally calcified vessels)
- 1.0–1.30 = normal value
- 0.91–0.99 = borderline
- 0.40– 0.90 = mild to moderate PAD → claudication
- < 0.40 = severe PAD → resting pain, gangrene (critical limb ischemia)
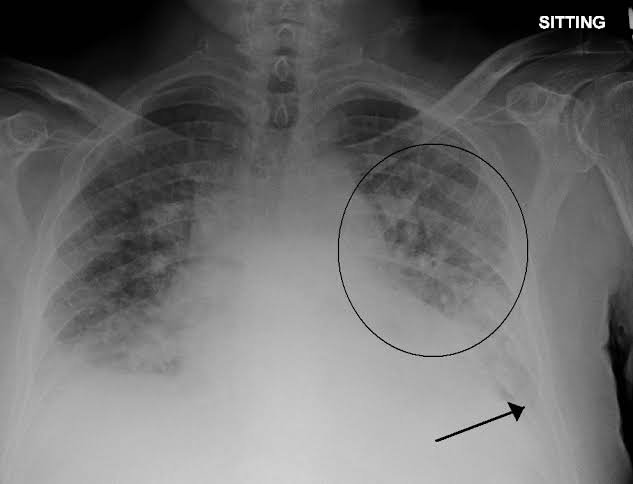
Imaging
- Color-coded duplex ultrasonography
- Digital subtraction angiography (DSA): Gold standard. Highest diagnostic accuracy, real-time visualization of arteries but exposes patients to intravenous contrast agents and radiation.
- CT angiography
- MR angiography
- Oscillography
Treatment
Conservative
- Smoking cessation!
- Supervised graded exercise therapy
- Foot care (especially in diabetic patients)
- Avoid cold temperatures
Medical
- Antiplatelet therapy reduces morbidity and mortality
- Aspirin: irreversible cyclooxygenase inhibition → decreased thromboxane A2 synthesis → decreased platelet aggregationADP receptor inhibitors
- Clopidogrel: inhibition of the P2Y12 ADP receptor → decreased platelet activation and platelet-fibrin crosslinking
- Ticagrelor: reversible inhibition of the P2Y12 ADP receptor (otherwise identical downstream effects as clopidogrel)
- Lipid-lowering agent (usually statins)
- Antihypertensive treatment
- Hyperglycemia control
- PDE inhibitors
- Cilostazol (the single most effective medication) – It is indicated in patients with lifestyle-limiting intermittent claudication only after 3 months of supervised graded exercise
- Mechanisms
- Phosphodiesterase 3 (PDE3) inhibition → increased cAMP → increased activity of protein kinase A → reduced platelet aggregation
Revascularization
- Indications
- Critical limb ischemia
- Failure of conservative and pharmacologic treatment
- Inability to perform normal work or activities because of claudication
- No limitations to exercise by other disease (e.g., chronic heart failure) if claudication is improved
- Anatomy of the lesion allows low-risk and long-term success of intervention
- Minimally invasive interventional radiology: percutaneous transluminal angioplasty (PTA) with or without stenting
-
- Operative vascular reconstruction (bypass surgery): an autologous vein (e.g., great saphenous vein) is used to bypass the stenosis
- Endarterectomy