The sudden death of an infant under 1 year of age, which remains unexplained after a thorough case investigation, including performance of a complete autopsy, examination of the death scene, and a review of the clinical history.
Epidemiology
- Peak incidence: 2–6 months, in rare cases, during the first days of life
- Sex: Male> Female
Etiology
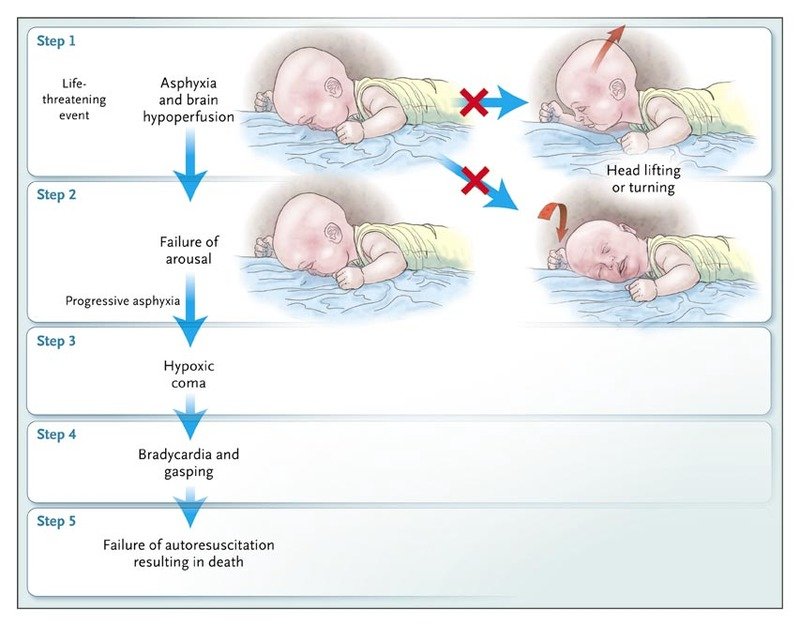
Aetiology is currently unknown. Indeed, the identification of a specific aetiology/acute process in an infant as a cause of death is sufficient to eliminate the diagnosis of SIDS. Evidence suggests that it is caused by a combination of both extrinsic and intrinsic factors, which ultimately lead to acute or chronic hypoxia. Over 90% of cases of SIDS occur during sleep.
Extrinsic factors (triggers)
- Sleeping in the prone position
- Exposure to nicotine during pregnancy and after birth (including 2nd-hand smoking)
- Overheating
- Unsafe sleeping environment or CO2 rebreathing: e.g., a shared blanket, stuffed animals in the crib (because of the grasping reflex, newborns tend to drag items to their faces)
- Many more correlations: SIDS in siblings, babies born prematurely, young mothers (< 16 years), low socioeconomic status, etc
Intrinsic factors
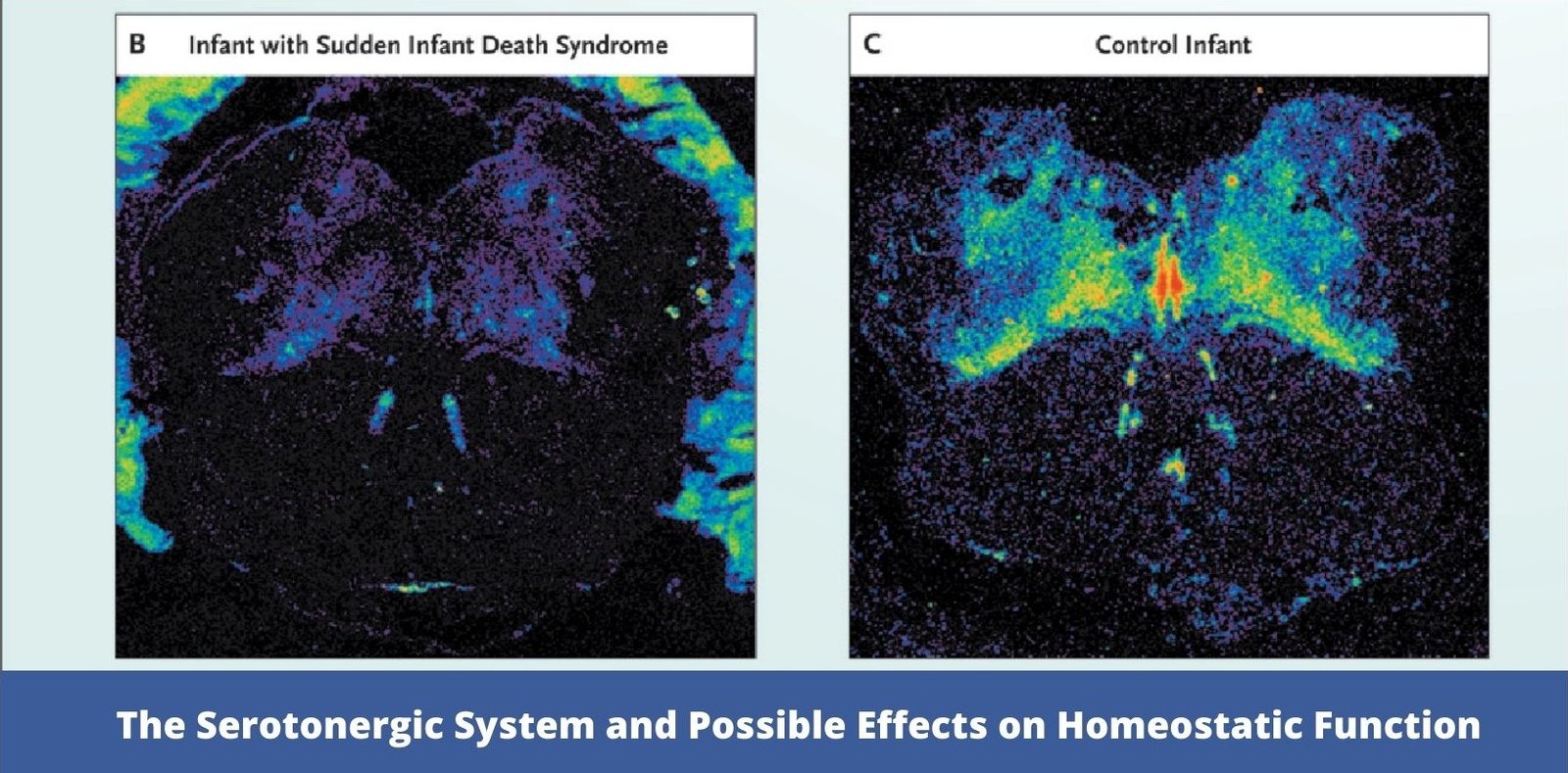
- Brainstem disorder that includes morphologic/biochemical abnormalities of serotonin (known as 5-hydroxytryptamine or 5-HT), which impacts the respiratory drive, the ability to wake up, blood pressure, upper respiratory reflexes and body temperature
- Mutations in genes encoding for Na+ or K+ channels linked to long QT syndrome have been reported in 5% to 29% of SIDS victims. Although this percentage is significantly higher than that observed in the general population, dysrhythmias appear to account for only 5% to 10% of deaths from SIDS
Differential diagnosis
SIDS is a diagnosis of exclusion. If there is an unexplained death of an apparently healthy infant, an autopsy is required by law to rule out other causes of death.
- Congenital anomalies that could lead to infant death (e.g., cardiac anomalies)
- Intentional suffocation; evidence of battered child syndrome
Prevention
- Avoidance of antenatal and postnatal smoke exposure
- The infant should be placed to sleep in the supine position
- Safe sleep environment: firm mattress; no pillows, blankets, stuffed animals, or bumper pads in the crib
- In the first 6 months, co-sleeping in the same room without bed-sharing
- Breastfeeding should be encouraged during the first 6 months of life
- Putting the baby in a prone position during playtime helps to strengthen neck muscles. If the baby then rolls onto the belly while sleeping, the baby will then be more likely to place his or her head in a safe position (that does not obstruct the airway)
- Immunization in line with the official schedule