INTRODUCTION
PATHOPHYSIOLOGY
CAUSES
History of hormone replacement therapy
Parimenopausal women in their child bearing ages are at risk of developing Systemic Lupus Erythematosus. Males with Klinefelter’s syndrome also at risk of developing this condition campare to normal males. Hormone replacement therapy is known to induce flareups.
Drug history
Some drugs like hydralazine, isoniazid, procainamide, penicillamine can induce this condition.
History of exposure to sun light
Ultraviolet light is a known triggering factor.
History of recent Epstein–Barr virus infection
Exposure to Epstein–Barr virus also a known predisposing factor.
Family history of diagnosed SLE or feature suggestive of SLE
Systemic Lupus Erythematosus goes as a hereditory disease. Deficiencies of the complement genes C1q, C2 or C4 are at risk of developing Systemic Lupus Erythematosus.
Past medical history
In a diagnosed patient complete past medical history will be useful in further management. About previous episodes, complications, tratments given, medications which patient is currently on.
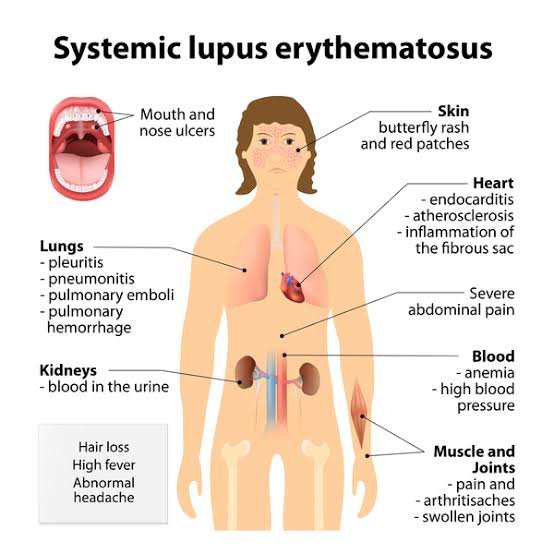
CLINICAL FEATURES
INVESTIGATIONS
-
Full blood countpatients can develop neutropenia, lymphopenia, thrombocytopenia and anaemia (Anaemia of chronic disease or autoimmune haemolytic anaemia).
-
ESR, CRPIn a controlled disease ESR will be high but CRP will be normal. But if there is any active inflammatory condition is present, CRP will be high.
-
Autoantibodies like ANA, anti-dsDNA, anti-Ro, anti-Sm and anti-LaThere are several antibodies present in Systemic Lupus Erythematosus. ANA are positive in more than 95% of patients.
-
Serum complement C3 and C4 levelsThese are normal during the remission but levels are low during flareups.
-
Renal function tests like UFR, serum creatinine, blood uresThese tests help in diagnosing the renal involvement.
-
Liver function tests like AST, ALT, serum billirubin, serum albumin level and Ultrasound scan of the abdomenLiver function tests helpful in diagnosing the liver involvement and Ultrasound scan of the abdomen will help to assess the presence of ascitis.
-
ECG, EchocardiogramThese will be helpful in diagnosing the cardiovascular complications like pericardial effusions, arrhythmias, and valvular abnormalities.
-
Chest X rayAs Systemic Lupus Erythematosus can cause pulmonary involvement, Chest X ray is useful.
-
CT/ MRI scan of brainThese tests will be useful in assessing cerebral complications. Brain arophy, brain infarction following vasculitis can be identified
-
Pleural aspirates for cytology, culture and ABSTIn the presence of pleural effusion these tests useful in identifyint the exudate anfd excluding pulmonary infections.
-
Histological and immunofluorescent study of biopsies from the kidney and the skinIn these studies deposition of IgG and complement will be identified. This will be useful in classifying the lupus nephritis as well.
-
CSF studies like CSF full report, culture and ABSTThese will be helpful in excluding the septic meningitis in patients with clinical symptoms and signd suggestive of meningit
MANAGEMENT
-
Health educationPatient should be educated regarding the disease, symptoms associated with, possible complications, investigations needed, available treatment options, predisposing factors for exacerbations and prognosis. As this is a life long genetically transmitting disease that fact also need to be address.
-
Life style modificationDue to the symptoms associated with the disease patient’s normal day to day life can be affected. eg: malaise, lethargy, fatiguability will limit the patient to bed. Joint pain and deformities will interfere with fine works. This should be discussed with the patient and physiotherapy, occupational therapy and help from social services can be afforded to improve the quality of life.
-
Avoid precipitating factorsPatient should be provide informations regarding precipitating factors like excessive exposure to sun light, drugs causing exacerbations and hormone replacement therapy. These factors should be avoided (eg: use high factor sun blocks to minimize UV light exposure) as much as possible and patient should be educated to early identification of exacerbations.
-
Non Steroid Anti Inflammatory DrugsIn the presence of arthralgia, arthritis, serositis, fever and other constitutional symptoms standard doses of Non Steroid Anti Inflammatory Drugs will be useful.
-
Topical corticosteroidsTopical corticosteroids are helpful in managing the skin conditions in cutaneous lupus.
-
Antimalarial drugsAntimalarial drugs like chloroquine, hydroxychloroquine can be used in mild skin disease, fatigue and arthralgias where those symptoms cannot be controlled with NSAIDs.
-
CorticosteroidsVarious types of corticosteroids can be use to treat this condition. eg: Short course of oral corticosteroids in mild to moderate disease condition like presence of rash, serositis. Single intramuscular injections of long-acting corticosteroids or short courses of oral corticosteroids are useful in treating severe flares of arthritis, pleuritis or pericarditis. High dose of oral corticosteroids in lupus nephritis, cerebral lupus, severe haemolytic anaemia or thrombocytopenia.
-
Immunosuppressive drugsin addition to high dose of oral corticosteroids in lupus nephritis and cerebral lupus patients should be treated with immunosuppressive drugs like Cyclophosphamide, mycophenolate mofetil. Azathioprine like immunosuppressive drugs are used in maintaining remissions.
-
Newer drugs like rituximabThese are used in refractory cases of Systemic Lupus Erythematosus. It reduces the auto antibody levels by suppressing levels of CD20 positive B lymphocytes.
-
WarfarinPatients with past history of previous thrombotic complications should be given life-long warfarin.
-
Management of pregnancy In Systemic Lupus ErythematosusAs mentioned above multidisciplinary team management should be considered. Pre- pregnant counseling about maternal risks (eg; increased risk of flareup, risk of development of hypertension, pre-eclampsia, placental abruption) and foetal risk (eg: pre term deliverty, pre term rupture of membranes, intra uterine growth retardation, intra uterine foetal death and development of neonatal lpus syndrome). advice to conceive during remissions as there is less risk of flare up. Treat hypertension and closely monitor for the foetures of pre eclampsis and imminent eclampsia. Treat flare ups similer to non pregnant state. advice patients not to stop hydroxychloroquine if patient is already on, as it can precipitate flare up. Manage the pregnancy in a hospital with tertiary care facilities available. closely monitor maternal and foetal well being.