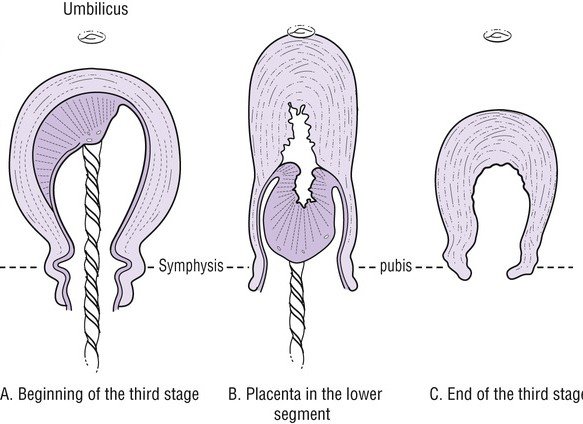
This is the most crucial stage of labor. Because most of the complications happen due to improper management in the third stage of the labor. Postpartum hemorrhage is a potentially life-threatening complication that persists as a leading cause of maternal death. It occurs mostly during the third stage of labor, and active management of the third stage of labor (AMTSL) can prevent its occurrence.
Third stage labor– Begins after the delivery of the baby and end at delivery of placenta. Main event in 3rd stage of labor is Delivery of placenta.
Advantages
- Duration: 5-10 min
- Bleeding: Decreased
- PPH and maternal mortality: Decreased
Steps
- Administration of uterotonic agents after delivery of the baby
- Expulsion of placenta with controlled cord traction
- Uterine fundal message after expulsion of placenta
1. Administration Uterotonic agents
- Enhance contraction of the uterus
- Facilitate expulsion of the placenta
- Decrease blood loss
Oxytocin–
Dose: 10 IU (I.M or I.V infusion). It is the drug of choice.
Importance: Oxytocin is the most commonly used agent and the primary drug of choice. Oxytocin can be used just after delivery of the front shoulder of the baby or expulsion of the placenta. Generally, its administration route and dose are 10 IU intramuscularly (IM). It can also be used intravenously (IV), which is typically preferred during cesarean sections (CS). Oxytocin also decreased postpartum blood loss when applied inside the placental cord
Methylergometrin (Methergine)–
Dose: 0.2mg (I.M)
Importance: Ergometrine causes continuous contraction of the uterus. There is not enough evidence about its use as a single agent. It is typically administered at 0.2 mg IM. Its use must be avoided in patients with hypertension.
Syntometrine–
Dose: 5U oxytocin + 0.5mg methylergometrine
Importance: This contains 5 IU oxytocin and 0.5 mg ergometrine. The time of onset of the uterine response after IM administration is shorter than after ergometrine alone, and the duration of action is several hours. Although it was found to be more effective than oxytocin
Carbitocin–
Dose: 100mcg (slow I.V)
Importnace: Carbetocin, given 100 μg as an IV bolus over 1 minute, instead of continuous oxytocin infusion, can be administered in elective caesarean section for the prevention of PPH, in the attempt to decrease the need for therapeutic uterotonics.
Carboprost–
Dose: 250mcg (I.M)
Importance: Carboprost is a synthetic prostaglandin analogue of PGF2α. Carboprost main use is in the obstetrical emergency of postpartum hemorrhage which reduces postpartum bleeding.
2. Controlled Cord Traction (CCT)
- Technique to assist in expulsion of placenta.
- Delayed cord clamping
- Helps to reduce the chances of a retained placenta and subsequent bleeding i.e. PPH.
- More than equal to 1min to 3min after delivery baby
Controlled umbilical cord traction (Brandt-Andrews maneuver)-
- One hand is placed on the abdomen, securing the uterine fundus and preventing uterine inversion.
- The other hand applies steady downward traction on the umbilical cord.
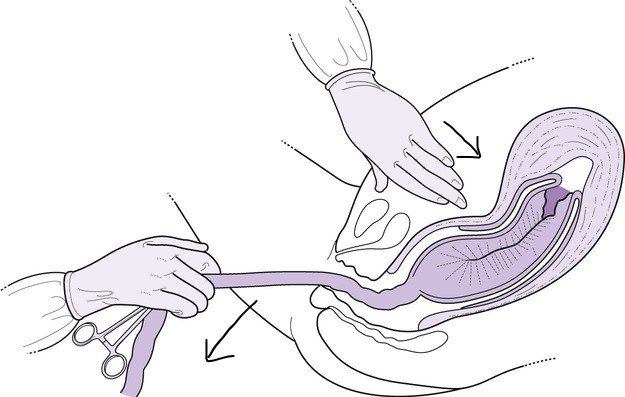
Never apply cord traction (pull) without a contraction and without applying countertraction (push) above the pubic symphysis with the other hand.
3. Uterine fundal massage
- Immediately after delivery of the placenta
- Helps in contraction of the uterus and thus
prevents PPH
Bimanual uterine massage is often adequate. The most commonly used techniques are Fritsch maneuver and Credé maneuver.
- A clenched fist is inserted into the anterior vaginal fornix and exerts pressure on the anterior wall of the uterus.
- The other hand is positioned externally and presses against the inner fist, located in the uterine body.

Uterine fundal massage after placental expulsion provides uterine contractions by stimulating endogenous prostaglandin secretion. This method was recommended in the 2007 WHO guidelines, and was described as optional for the active management of the third stage in the 2012 updated guidelines.
Adverse effects of active management
- Adverse effects related to uterotonic agents
- Hypertension, nausea, vomiting due to ergot alkaloids
- Risk of placental retention
- Neonatal risks related to early cord clamping
- Iron-deficiency anemia
- Intraventricular hemorrhage
- Hypotension