Paroxysmal nocturnal hemoglobinuria (PNH) is a rare acquired disorder characterized by a triad of hemolytic anemia, pancytopenia, and thrombosis.
Why this Name?
The name paroxysmal nocturnal hemoglobinuria comes from:
- Paroxysmal – means “sudden and irregular”
- Nocturnal – means “at night”
- Hemoglobinuria – means “hemoglobin in urine”; hemoglobin, the red part of red blood cells, makes urine look dark
So, “paroxysmal nocturnal hemoglobinuria” means sudden, irregular episodes of passing dark colored urine, especially at night or in the early morning. It is important to note this can be a bit misleading, because many people with PNH do not have dark urine.
Incidence
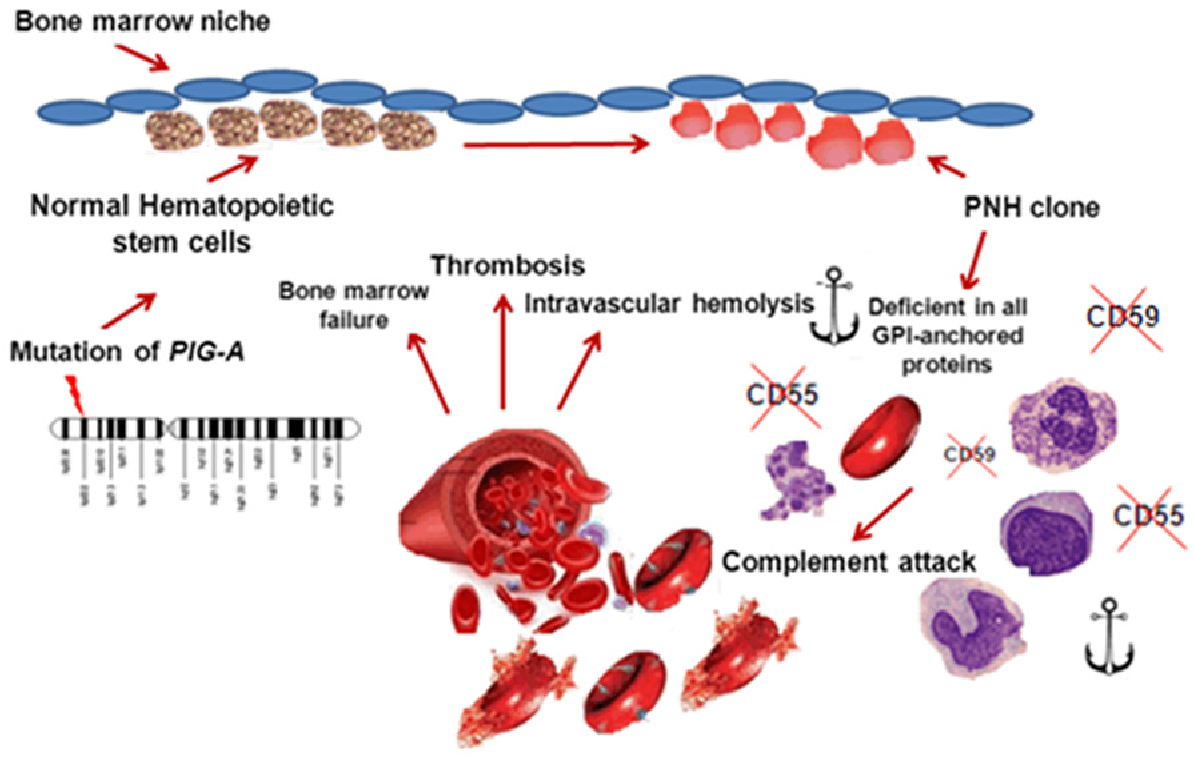
Both arterial and venous thrombosis can occur in the extremities as well as in less common sites such as portal veins and cerebral venous sinuses. Thrombosis is a result of increased complement activation and hemolysis. Protracted urinary hemoglobin loss may result in iron deficiency. Paroxysmal nocturnal hemoglobinuria is associated with bone marrow dysfunction, likely due to immunologic attack on hematopoietic stem cells, often leading to leukopenia and thrombocytopenia. About 20% of patients with severe aplastic anemia, another clonal hematopoietic disorder, have a detectable PNH clone.
Pathophysiology
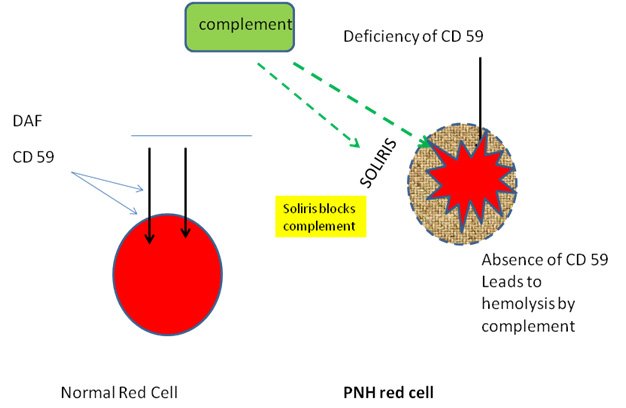
- Physiologically, a membrane-bound glycosylphosphatidylinositol (GPI) anchor protects RBCs against complement mediated hemolysis.
- Acquired mutation on the PIGA gene located on the X chromosome → GPI anchor loses its protective effect → RBC destruction by complement and reticuloendothelial system → intravascular and extravascular hemolysis
- The GPI anchor proteins involved in PNH are:
- CD55/DAF (Decay accelerating factor)
- CD59/MIRL (Membrane inhibitor of reactive lysis)
- PNH can also occur in patients with aplastic anemia
Clinical symptoms
Due to the wide spectrum of symptoms associated with PNH, it is not unusual for months or years to pass before the correct diagnosis is established. Overall, the most common symptoms of PNH include:
- Pallor, excessive fatigue, weakness
- Bruising or bleeding easily
- Shortness of breath
- Intermittent jaundice
- Episodes of hemoglobinuria causing pink/red/dark urine which usually occurs in the morning due to concentration of urine overnight.
- Venous thrombosis in unusual locations e.g., hepatic, cerebral, and/or abdominal veins
- Vasoconstriction
- Headache, pulmonary hypertension
- Abdominal pain, dysphagia, erectile dysfunction
- Increased risk of infections (in case of pancytopenia)
Diagnosis
- CBC: anemia or pancytopenia
- Flow cytometry: absence of CD55 and CD59 on RBC surface. This test is highly sensitive and specific.
- Coombs test: negative (Hemolysis in PNH is due to complement mediated RBC destruction and not due to antibodies)
- Serum studies: decreased levels of haptoglobin
Treatment
- Prednisone for initial therapy
- Eculizumab(Soliris): anti-C5 antibody (complement inhibitor)
- Bone marrow transplantation: in case of bone marrow hypoplasia
- Allogeneic stem cell transplantation
- Iron and folate supplementation
Complications
- Vasoconstriction and thrombotic emboli leading to thrombotic complications, e.g., infarctions, Budd-Chiari syndrome
- Increased risk of acute leukemias