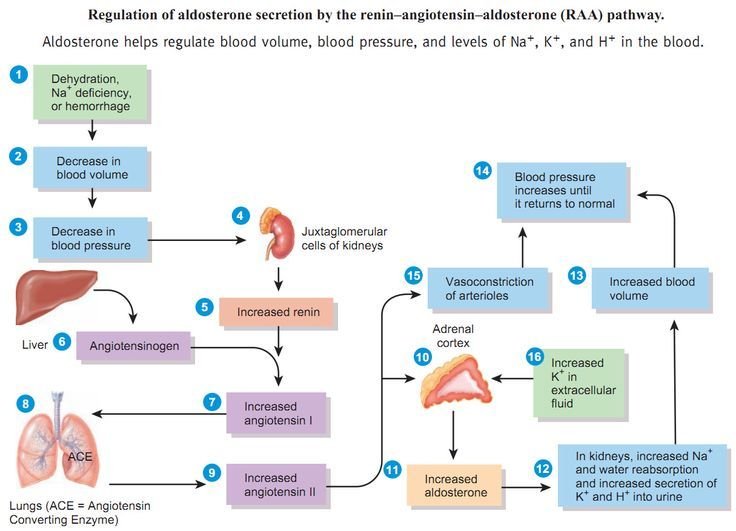
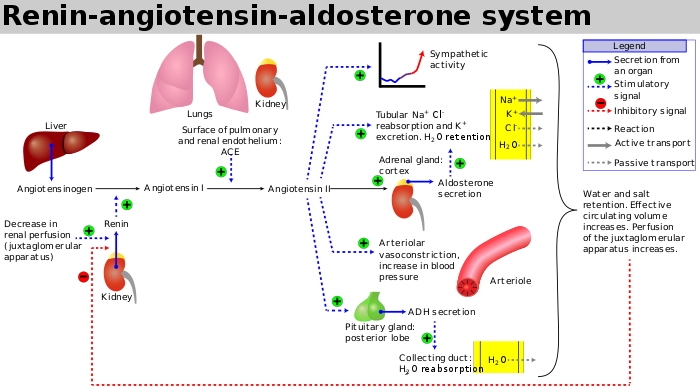
Renin angiotensin aldosterone system
The renin-angiotensin-aldosterone system (RAAS) plays an important role in regulating blood volume and systemic vascular resistance, which together influence cardiac output and arterial pressure. As the name implies, there are three important components to this system: 1) renin, 2) angiotensin, and 3) aldosterone.
Renin
Renin, which is released primarily by the kidneys, stimulates the formation of angiotensin in blood and tissues, which in turn stimulates the release of aldosterone from the adrenal cortex.
Renin is a proteolytic enzyme that is released into the circulation by the kidneys. Its release is stimulated by:
- Sympathetic nerve activation (acting through β1-adrenoceptors)
- Renal artery hypotension (caused by systemic hypotension or renal artery stenosis)
- Decreased sodium delivery to the distal tubules of the kidney.
♦Renin-angiotensin-aldosterone system regulating arterial pressure♦
Mechanism
Juxtaglomerular (JG) cells associated with the afferent arteriole entering the renal glomerulus are the primary site of renin storage and release. A reduction in afferent arteriole pressure causes the release of renin from the JG cells, whereas increased pressure inhibits renin release.
Beta1-adrenoceptors located on the JG cells respond to sympathetic nerve stimulation by releasing renin. Specialized cells (macula densa) of distal tubules lie adjacent to the JG cells of the afferent arteriole. The macula densa senses the concentration of sodium and chloride ions in the tubular fluid. When NaCl is elevated in the tubular fluid, renin release is inhibited. In contrast, a reduction in tubular NaCl stimulates renin release by the JG cells. There is evidence that prostaglandins (PGE2 and PGI2) stimulate renin release in response to reduced NaCl transport across the macula densa.
When afferent arteriole pressure is reduced, glomerular filtration decreases, and this reduces NaCl in the distal tubule. This serves as an important mechanism contributing to the release of renin when there is afferent arteriole hypotension, which can be caused by systemic hypotension or narrowing (stenosis) of the renal artery that supplies blood flow to the kidney.
When renin is released into the blood, it acts upon a circulating substrate, angiotensinogen, that undergoes proteolytic cleavage to form the decapeptide angiotensin I. Vascular endothelium, particularly in the lungs, has an enzyme, angiotensin converting enzyme (ACE), that cleaves off two amino acids to form the octapeptide, angiotensin II (AII), although many other tissues in the body (heart, brain, vascular) also can form AII.
Angiotensin II has several very important functions:
- Constricts resistance vessels (via AII [AT1] receptors) thereby increasing systemic vascular resistance and arterial pressure
- Stimulates sodium transport (reabsorption) at several renal tubular sites, thereby increasing sodium and water retention by the body
- Acts on the adrenal cortex to release aldosterone, which in turn acts on the kidneys to increase sodium and fluid retention
- Stimulates the release of vasopressin (antidiuretic hormone, ADH) from the posterior pituitary, which increases fluid retention by the kidneys
- Stimulates thirst centers within the brain
- Facilitates norepinephrine release from sympathetic nerve endings and inhibits norepinephrine re-uptake by nerve endings, thereby enhancing sympathetic adrenergic function
- Stimulates cardiac hypertrophy and vascular hypertrophy
The renin-angiotensin-aldosterone pathway is not only regulated by the mechanisms that stimulate renin release, but it is also modulated by natriuretic peptides released by the heart. These natriuretic peptides acts as an important counter-regulatory system.