Urticaria is a disease characterized by erythematous, edematous, itchy and transient plaques, that involve skin and mucous membranes.
Epidemiology
It can be seen in all ages and sexes but is slightly more common in young adults. In 40–50% of the patients, urticaria and angioedema are seen in combination, only urticaria or angioedema is seen in 40% and 20% of the people, respectively.
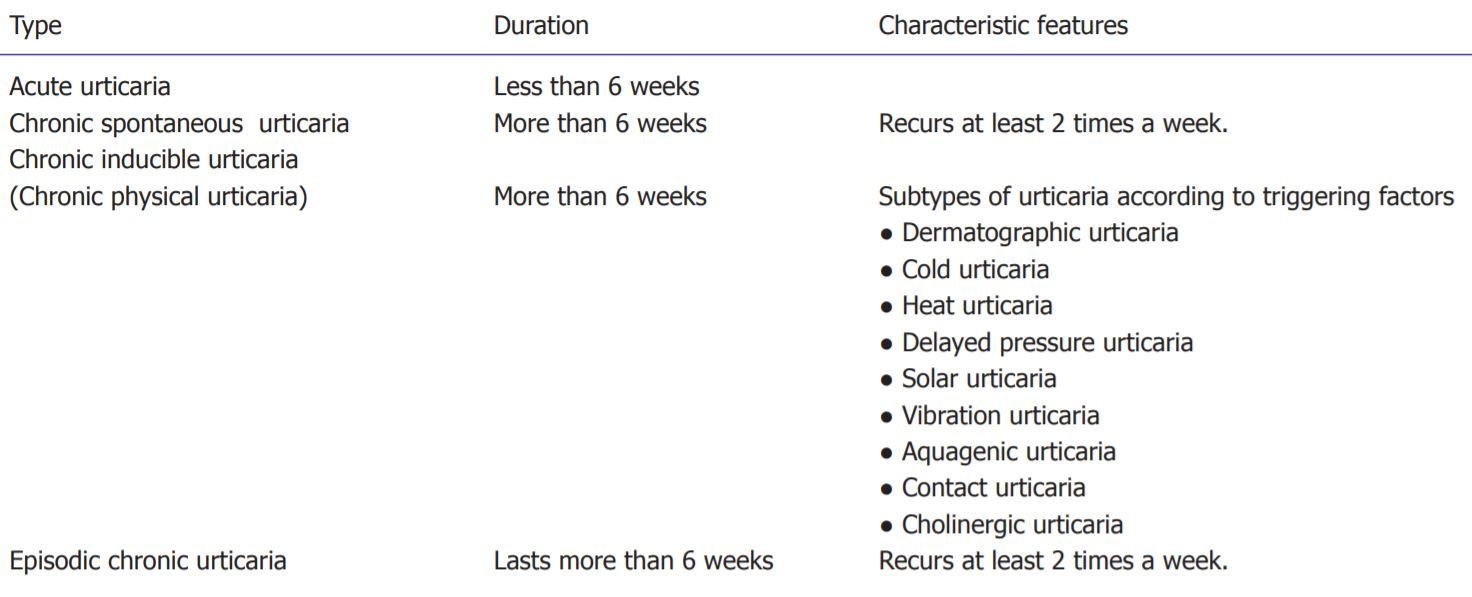
Classification
Pathogenesis
The main mechanism in the formation of urticaria is the release of various mediators from mast cells. Type 1 immunoglobulin (Ig) E dependent hypersensitivity reaction is seen in acute urticaria. The antigen entering the body binds to specific antibodies on mast cells and basophils, causing the release of many mediators, primarily histamine. As a result, edema occurs due to erythema and increased permeability secondary to vasodilatation. Mast cells cannot be restimulated until regranulation after degranulation, which explains why the urticaria does not reappear for several days on the region. In chronic urticaria, the antigen entering the body binds to the IgE high affinity (FceRIa) Fc receptor located on the mast cells and circulating basophils in the skin and degranulation from these cells occurs. When the same antigen is encountered for the 2nd time, these IgE antibodies that are already present on the mast cells and basophils immediately bind to the antigen and develop an allergic reaction more quickly. This shows us that autoimmunity is also important in chronic urticaria.
Etiology
Hives and angioedema can be caused by:
- Foods – Many foods can trigger reactions in people with sensitivities. Shellfish, fish, peanuts, tree nuts, soy, wheat, eggs and milk are frequent offenders.
- Medications – Many medications may cause hives or angioedema. Common culprits include penicillin, aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and blood pressure medications.
- Airborne allergens – Pollen and other allergens that you breathe in can trigger hives, sometimes accompanied by upper and lower respiratory tract symptoms.
- Environmental factors – Examples include sunlight, vibration such as from using a lawn mower, hot showers or baths, pressure on the skin such as from tight clothing or scratching, emotional stress, insect bites and exercise.
- Medical treatments or underlying conditions. Hives and angioedema also occasionally occur in response to blood transfusions and infections with bacteria or viruses such as hepatitis and HIV.
- Oftentimes, no specific cause can be identified, especially in the case of chronic hives.
Clinical Features
- The urticarial plaque has three characteristics as characteristic redness, blistering, and itching. Sometimes, a burning sensation.
- Lesions can occur anywhere in the body and recover in approximately 2–3 h without leaving a trace. This spontaneous recovery can sometimes last up to 1 day.
- In angioedema, there are swelling and redness, especially around the eyes, cheeks or lips. The lesions regress spontaneously in about 72 h.

Diagnosis
Diagnosis based on clinical features and patients’ history. If there is any exposure of pollens, food intake or medications. There is no need for routine laboratory tests and allergy tests in acute urticaria. In a guideline published in the United States, it has been reported that if there is no evidence to support a diagnosis, then there is no need for laboratory examinations.
Treatment
The first thing is Prevention.
- Avoid known triggers. If you know what triggered your hives, try to avoid that substance.
- Bathe and change your clothes. If pollen or animal contact has triggered your hives in the past, take a bath or shower and change your clothes if you’re exposed to pollen or animals.
In the treatment of urticaria (with or without angioedema), the focus should be on the immediate relief of pruritus and angioedema, if any. Approximately two-thirds of the cases of acute urticaria may be spontaneously confined and recover spontaneously. If there are any exaggerated situations occur then medications used in the treatment are.
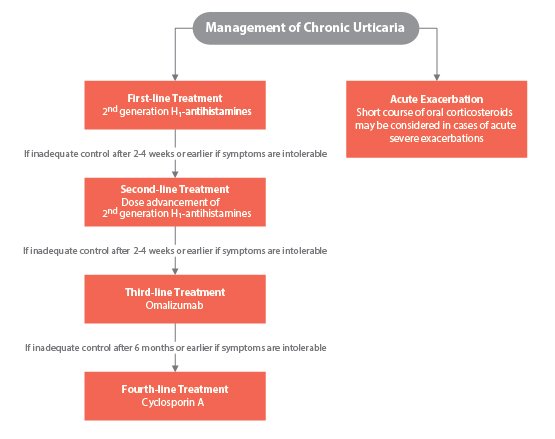
H1 antihistamines
Antihistamines bind to histamine receptors and prevent the formation of pruritus and urticarial plaques. Mainly use 2nd generation agents like cetirizine, loratadine, fexofenadine, desloratadine, levocetirizine etc.
Systemic corticosteroids
Glucocorticoids do not inhibit mast cell degranulation, but they probably act by suppressing various inflammatory mechanisms. However, systemic glucocorticoids should be considered in cases with significant angioedema or if the symptoms persist for more than a few days and cannot be controlled by antihistamines. In adults, prednisone is given for an average of 5–10 days at daily doses of 30–60.
Cyclosporine
Compared with systemic corticosteroids, cyclosporine has been reported to cause a more rapid and long-term remission.
Omalizumab
Omalizumab, a monoclonal antibody (anti-IgE IgG) against IgE, is safe and effective for many patients, but it is too expensive and does not appear to have long-term disease-improving effects. Omalizumab reduces mast cell function and induces eosinophil apoptosis. It reduces cytokine release from basophils and migration of immune cells to tissue.
Treatment of angioedema
Angioedema is not only seen as swelling in the skin and lips but sometimes also causes swelling in the tongue and larynx and may be life threatening. Therefore, treatment of angioedema is important. First of all, make sure that the patient’s airway is open and he/she is breathing comfortably. The standard treatment for patients without respiratory distress is H1 and H2 antihistamines and systemic corticosteroids. If the patient has airway constriction or hypotension, the epinephrine should be administered intramuscularly at a dose of 0.2–0.5 mg.
Ref : Asthma and Allery Foundation of America, BMJ