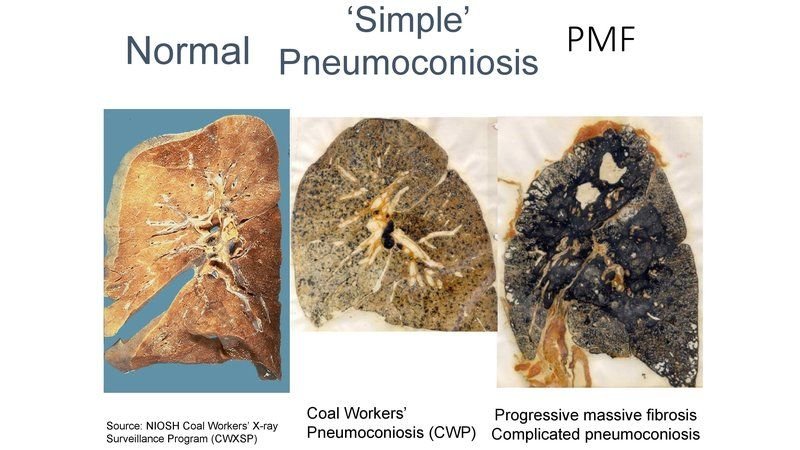
Pneumoconiosis is one of a group of interstitial lung disease caused by breathing in certain kinds of dust particles that damage your lungs. Due to the fact that people encounter these dusts only in the workplace, pneumoconiosis is called an occupational lung disease. Pneumoconiosis usually take years to develop. Because your lungs can’t get rid of all these dust particles, they cause inflammation in your lungs that can eventually lead to scar tissue.
The term pneumoconiosis derives its meaning from the Greek words: Pneuma = air and Konis = dust
PATHOGENESIS
For clinical pneumoconiosis to develop, 3 essential factors are required:
- Exposure to specific substance: Coal, appear relatively inert and may accumulate in considerable amounts with minimal tissue response; while silica and asbestos, have potent biologic effects
- Particles of appropriate size to be retained in lung (1-5μm)
- Exposure for a sufficient length of time (usually around 10 years)
- Possible additional effects of other irritants like smoking

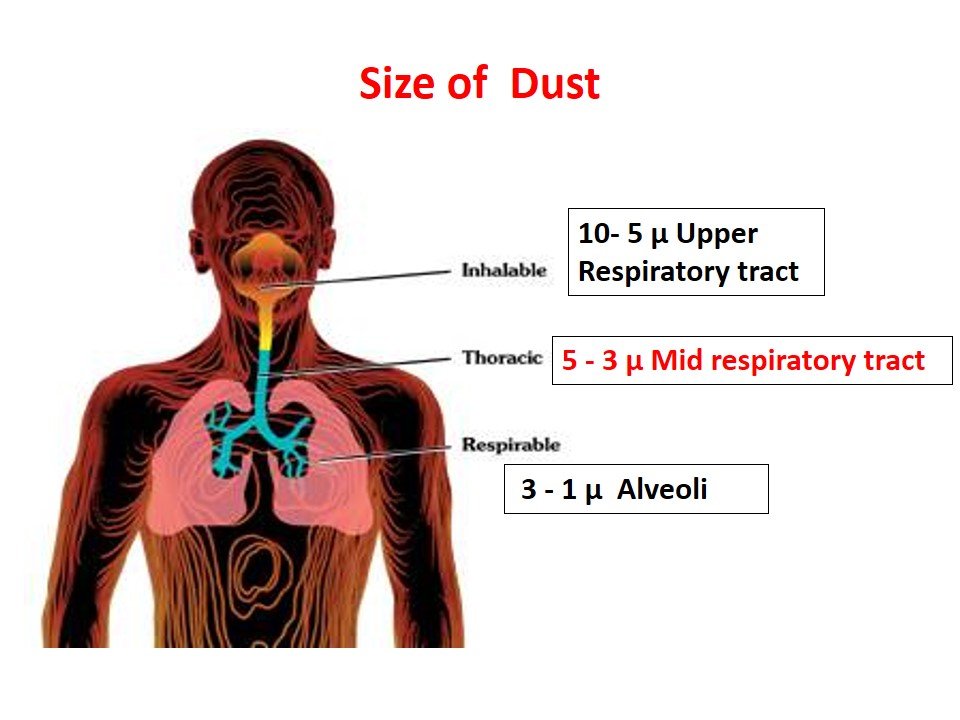
From an occupational health point of view, dust is classified by size into following categories:
- Inhalable Dust: It is the one which enters the body, but is trapped in upper respiratory tract. Particle size is usually 5-10μm. Can be expelled out by cough reflex.
- Respirable Dust: Particles that are small enough to penetrate the upper respiratory system and beyond the body’s natural clearance mechanisms by cough reflex are more likely to be retained in the mid respiratory tract. Particle size is usually 3-5μm.
- Particles of size 1-3μm deposited directly in the alveoli.
- Particles of <1 μm are move in and out of the alveoli with air
TYPES
Pneumoconiosis is usually divided into three groups:
- Major pneumoconiosis
- Minor pneumoconiosis
- Benign pneumoconiosis “ Fibrotic Pneumoconiosis”
1.Major Pneumoconiosis-
Inhalation of some dusts results in “major fibrosis” of the lungs, which results in interference of lung architecture or lung function tests.
Examples:
- Silica : Silicosis also k/a “grinder’s disease” or “Potter’s rot”
- Asbestos : Asbestosis
- Coal: Anthracosis also k/a “miner’s lung” or “black lung”
- Cotton: Byssinosis also k/a “brown lung”
2.Minor Pneumoconiosis-
Inhalation of some dusts results in “minor fibrosis” of the lungs. There is minimal fibrosis of the lungs without interference of lung architecture or lung function tests.
Example:
- Mica pneumoconiosis (Mica is a common mineral containing aluminum, iron, or magnesium silicates)
- Kaolin (china clay) pneumoconiosis
3.Benign Pneumoconiosis-
There isn’t any reaction in the lungs, but dust deposition casts a shadow in x-ray of the lung. There is no fibrosis and no disturbance of lung functions. They are characterized by the presence of small rounded dense opacities on a chest film due to perivascular collections of dusts. The deposits in the lung disappear when exposure is discontinued.
Examples:
- Iron dust : Siderosis
- Tin dust : Stannosis
- Calcium dust : Chalicosis (fine dust from stonecutting)
SYMPTOMS
Symptoms of pneumoconiosis often depend on how severe the disease is. Simple CWP (coal workers’ pneumoconiosis) may have no or few symptoms and show up only on an X-ray. PMF (Progressive massive fibrosis) may cause mild to severe difficulty breathing. Symptoms may include:
- Cough
- Lots of phlegm
- Shortness of breath
DIAGNOSIS
You may be diagnosed with pneumoconiosis if you have lung symptoms, X-ray abnormalities, and a history of working around coal, asbestos, or silica. You may also be diagnosed by having a routine X-ray during the time you are employed. The Federal Mine Safety and Health Acts require that all underground coal miners be offered a chest X-ray after three years and then at five-year intervals to look for the disease. Your doctor may use any of these to help make a diagnosis:
- Personal history of work exposure
- Physical examination
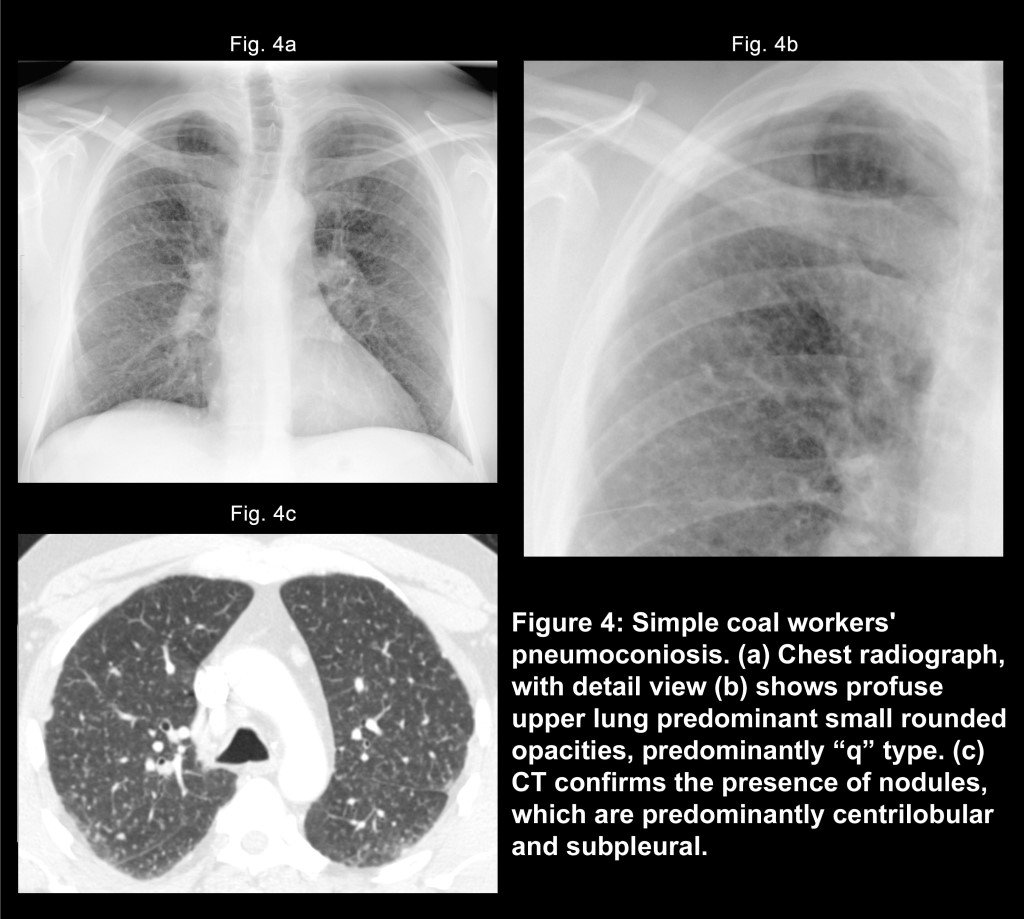
- Chest X-ray or CT scan to look for lung nodules, masses and interstitial disease
- CT scan of the chest
- Pulmonary function studies, including blood gasses
- Biopsy
TREATMENT
Pneumoconiosis can’t be cured. Once the disease has been diagnosed, treatment is aimed at keeping it from getting worse and controlling your symptoms. A treatment plan may include:
- Not smoking
- Avoiding all dust exposure
- Using oxygen
- Taking medications called bronchodilators that open lung passages
COMPLICATIONS
The main complication is when simple pneumoconiosis progresses to PMF. These are other possible complications:
- Progressive respiratory failure
- Lung cancer
- Tuberculosis (but this is now rare)
- Heart failure caused by pressure inside the lungs
PREVENTIVE MEASURES
Medical measures:
- Pre-placement examination
- Periodical examination
- Medical and health care services
- Notification
- Maintenance and analysis of records
- Health education and counselling
Practicing good personal hygiene:
- Washing hands and face before eating, drinking, going to the toilet, smoking.
- Do not eat, drink, smoke, or apply cosmetics in areas where silica is being used.
- Wear protective clothes and respiratory protection (Respirators must fit tightly.)
- Before leaving work, shower and change into clean clothes. Leave dusty clothes at work.
Engineering measures:
- Design of building
- Conduct air monitoring to measure the workers’ exposure to crystalline silica.
- Minimize exposures by controlling the creation of airborne particles, for example – use wet drilling, local exhaust ventilation.
- Personal Protective Equipment: Provide workers with protective clothes, respiratory protection, and facilities for washing (showers) and changing.
- Enclosure / isolation
- Environmental monitoring
Other measures:
- Legal measures: Measures to minimize dust emissions and exposure to dust.
- Law compliance mechanisms, including effective workplace inspection systems
- Cooperation between management and workers and their representatives
- A mechanism for the collection and analysis of data on occupational diseases
- Collaboration with social security schemes covering occupational injuries and diseases
- Training of health professionals in occupational diseases as majority of medical practitioners lack training in occupational health and consequently lack the skills to diagnose and prevent occupational diseases.