WOUND HEALING
A wound is a break in the integrity of the skin or tissues which may be associated with disruption of structure and function.
Rank and Wakefield classification
1. Tidy wounds
Inflicted by sharp instruments and contain no devitalised tissue; closed primarily with the expectation of quiet primary healing.
Examples are surgical incisions, cuts from glass and knife wounds.
Tendons, arteries and nerves will commonly be injured in tidy wounds, but repair of these structures is usually possible.
2. Untidy wounds
Result from crushing, tearing, avulsion, vascular injury or burns, and contain devitalised tissue.
Skin wounds will often be multiple and irregular.
Tendons, arteries and nerves may be exposed, and might be injured in continuity, but will usually not be divided. Fractures are common and may be multifragmentary.
Such wounds must not be closed primarily; if they are closed wound healing is unlikely to occur without complications. Pathophysiology in a diagram
HEALING
Healing is the body’s response to injury in attempt to restore normal function.
2 ways of healing
- REGENERATION : healing takes place by proliferation of parenchymal cells. Complete restoration occurs
- REPAIR: tissues do not return to their original architecture and function and results in scarring.
TYPES OF WOUND HEALING
HEALING BY PRIMARY INTENTION: wounds with opposed edges
- Clean and uninfected
- Surgically incised
- Wound with opposed edges
HEALING BY SECONDARY INTENTION: wounds with separated edges
- Extensive loss of cells and tissues
- Larger amount of granulation tissue formed
FACTORS AFFECTING WOUND HEALING
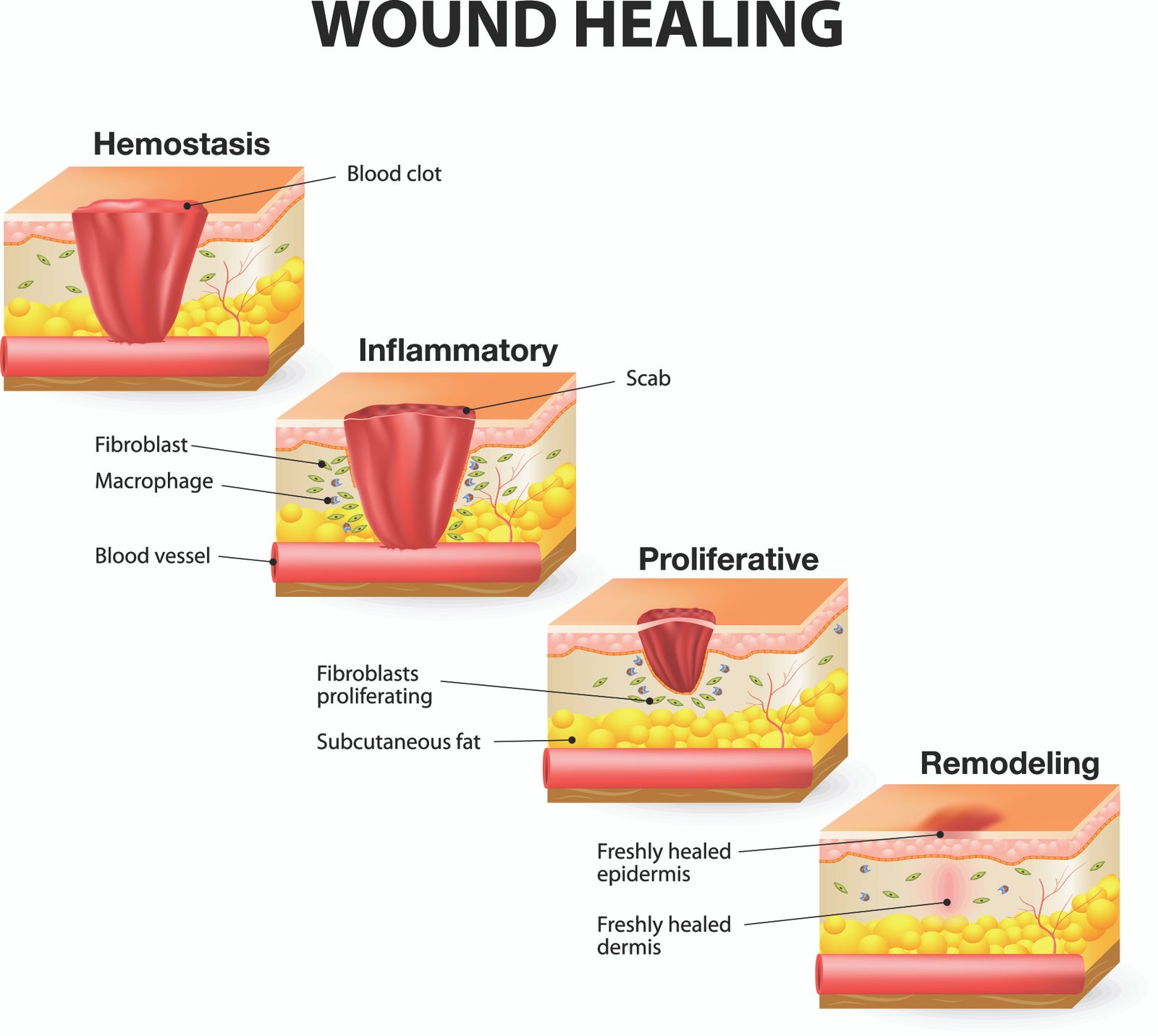
PHASES OF WOUND HEALING
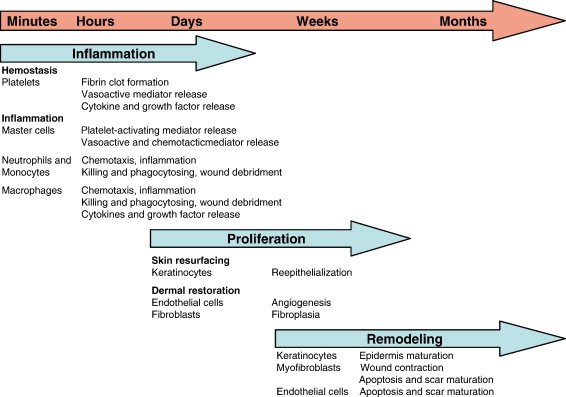
1. Inflammatory (up to 3 days after wound): Mediated by Platelets, neutrophils, macrophages – Clot formation,vessel permeability and neutrophil migration into tissue; macrophages clear debris 2 days later
2. Proliferative (day 3–weeks after wound): Mediated by Fibroblasts, myofibroblasts, endothelial cells, keratinocytes, macrophages – Deposition of granulation tissue and type III collagen, angiogenesis, epithelial cell proliferation, dissolution of clot, and wound contraction (mediated by myofibroblasts) Delayed second phase of wound healing in vitamin C and copper deficiency
3. Remodeling (1 week–6+ months after wound): Mediated by Fibroblasts – Type III collagen replaced by type I collagen, tensile strength of tissue Collagenases (require zinc to function) break down type III collagen Zinc deficiency delayed wound healing
4. Scar formation: Occurs when repair cannot be accomplished by cell regeneration alone. Nonregenerated cells (2° to severe acute or chronic injury) are replaced by connective tissue. 70–80% of tensile strength regained at 3 months; little tensile strength regained thereafter. Associated with excess TGF-β.
VARIOUS TISSUE MEDIATORS AND THEIR FUNCTIONS
- FGF : Stimulates angiogenesis
- TGF-β : Angiogenesis, fibrosis
- VEGF: Stimulates angiogenesis
- PDGF : Secreted by activated platelets and macrophages Induces vascular remodeling and smooth muscle cell migration Stimulates fibroblast growth for collagen synthesis
- Metalloproteinases : Tissue remodeling
- EGF : Stimulates cell growth via tyrosine kinases (eg, EGFR/ErbB1)