Acute Coronary Syndrome (ACS) is a broad topic caused by ischemia (and in some cases infarction) of myocardium (loss of blood supply to heart muscle). It is a medical emergency and required immediate hospital admission. We divide ACS by three terminology –
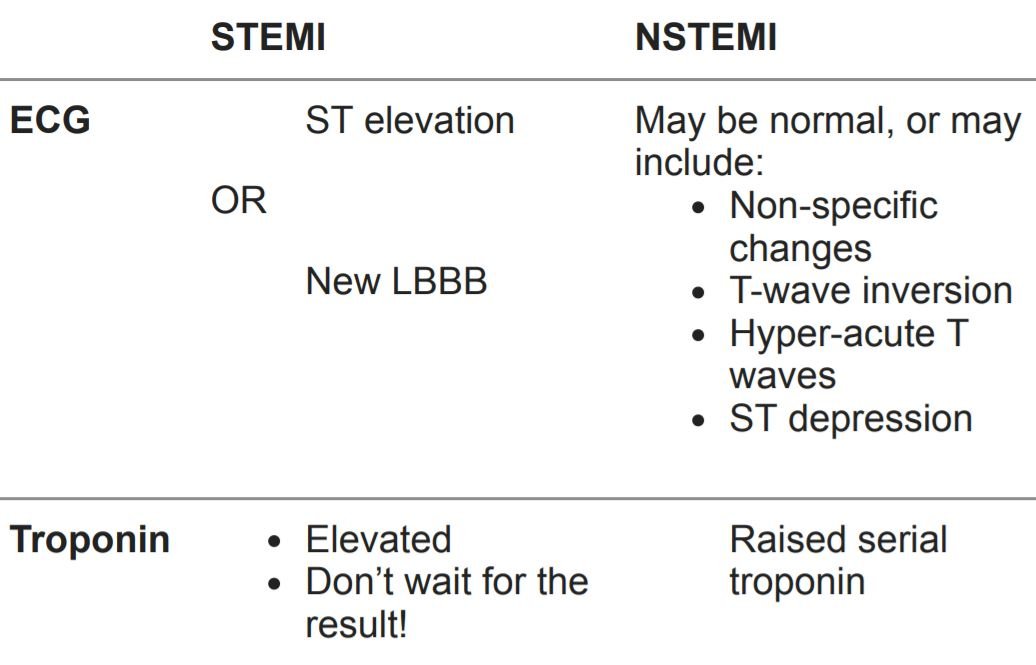
STEMI – ST elevation MI, Diagnosable on the basis of classical ECG changes
NSTEMI – Non-ST elevation MI, Usually diagnosed on the basis of a suggestive history, with positive biochemical markers – e.g. positive troponin
Unstable angina – Ischaemia, without infarction
They are grouped together because they all have a common mechanism – rupture
or erosion of the fibrous cap of a coronary artery plaque
Here we’ll discuss only about MI in brief, so that we can write in exam
So simply Myocardial Infarction means irreversible injury in cardiac tissue/complete occlusion of coronary artery/Necrosis of cardiac myocytes.
Causes
- Due to rupture of an atherosclerotic plaque with thrombosis and complete occlusion of coronary artery.
- Other causes: Coronary artery vasospasm (Due to Prinzmetal angina or cocaine use) , emboli and vasculitis.
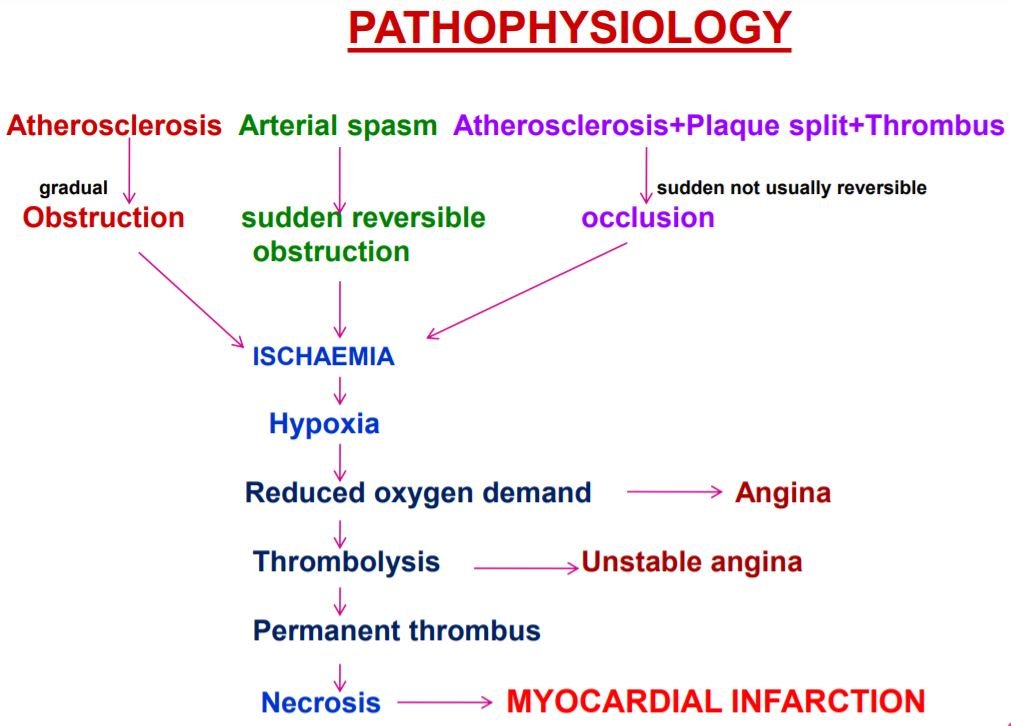
Pathophysiology
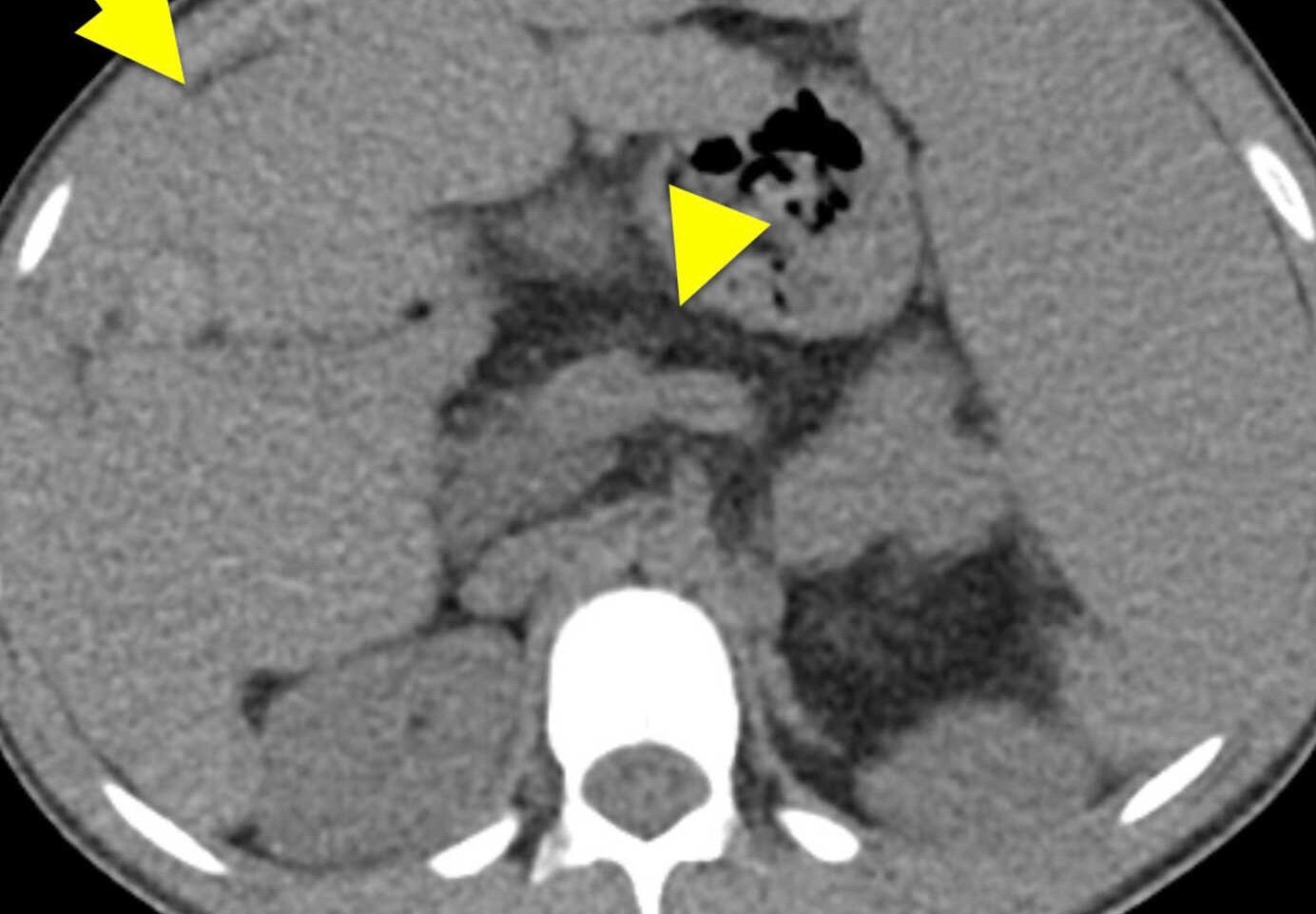
Ulceration/rupture of plaque → Spasm of coronary vessel. Here is graphical presentation below.
Localization of myocardial infarction ( ECG )
- Localization of ischemic area in ST Elevation Myocardial Infarction
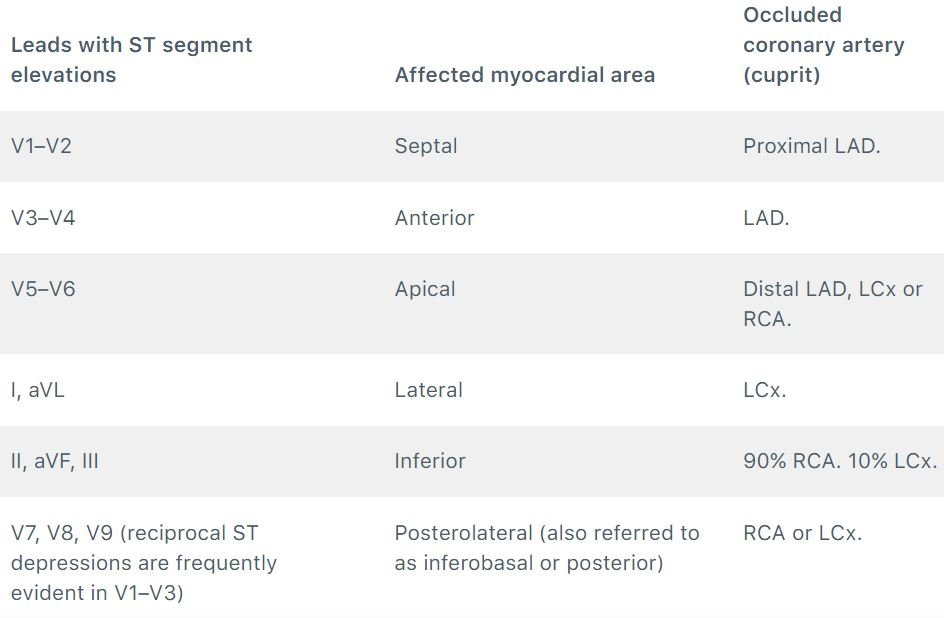
- Localizing the ischemic area in NSTE-ACS/NSTEMI is much more difficult because leads with ST-segment depressions do not reflect the ischemic area.
Occlusion in Coronary artery
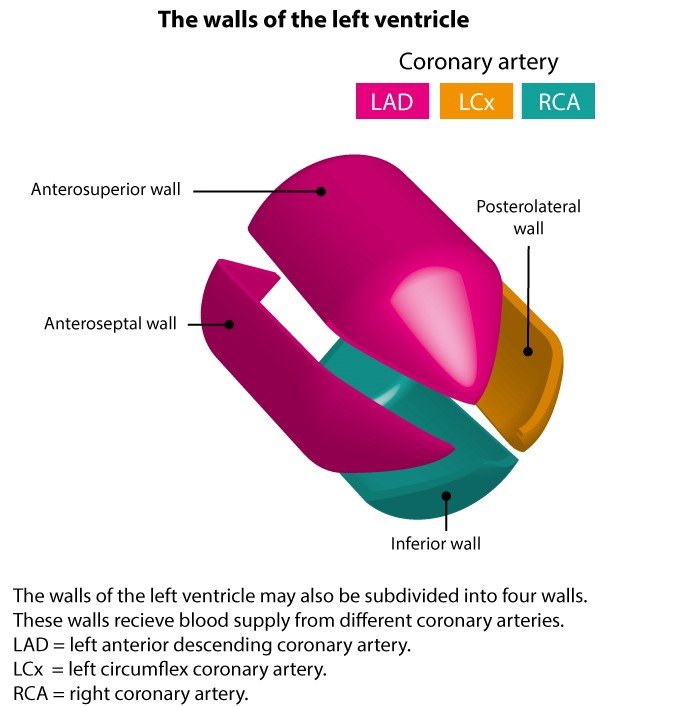
- Infarction usually involves Left ventricle, right ventricle. And both atria are generally spared.
- Occlusion of Left anterior descending artery (LAD) – Infarction of anterior wall and anterior septum of LV. Left anterior descending artery is the most commonly involved artery in MI.
- Occlusion of Right coronary (RCA) – Infarction of posterior wall, posterior septum and papillary muscles of the LV. Right coronary artery is the 2nd most commonly involved artery in MI.
- Occlusion of Left circumflex artery (LCA) leads to infarction of lateral wall of the LV.
Infarct extent
- Initial phase of infarction leads to Subendocardial necrosis involving <50% of the myocardial thickness. Usually characterized by abnormal Q waves on ECG.
- Continued or severe ischemia leads to Transmural necrosis involving most of the myocardial wall. EKG shows ST-segment elevation.
Clinical Manifestations
- Chest pain radiating to inner arm/jaw/epigastrium(No pain seen in elderly and DM patients). Typically a “crescendo pain” with increasing severity over a period of several minutes after onset
- Sweating – In this circumstance is often referred to as Diaphoresis
- Breathlessness
- Syncope – If this occurs, then it will be a result of severe arrhythmia, or severe hypotension
- Distress, also sometimes a ‘feeling of impending doom’
- Vomiting and sinus bradycardia – this may occur as a result of excessive vagal stimulation, which is most common in inferior MI
- Sudden death – this usually occurs from ventricular fibrillation or asystole
Signs
Signs of impaired myocardial function –
- 3 / 4 heart sounds
- Pan systolic murmur
- Pericardial rub
- Pulmonary edema – Crepitations in the lungs
- Hypotension
- Quiet first heart sound
- Narrow pulse pressure (difference of <40mmHg)
- Raised JVP
Signs of sympathetic activation –
- Pallor (basically looking pasty. It can be generalised or localised, but is only really
clinically significant if generalised. Most evident in the palms and on the face) - Sweating
- Tachycardia
Diagnosis
- Myoglobin: 1st enzyme to increase but non-specific.
- Creatine Kinase(CK-MB): Also increased in myocarditis.
- Troponin: Most specific and sensitive(also useful in diagnosis of Reinfarction).
- LDH: Last enzyme to increase.
- ECG: Hyper acute T waves.
- TTC+LDH: Useful to know cause of death at the time of autopsy.
- Echo: Hypokinesia.
- Thallium scan.
Here we’ll discuss about ECG Changes and Troponin tests with more details. But it’s not mandatory to write in details at exam. Read this two diagnostic procedure below to build up your concepts.
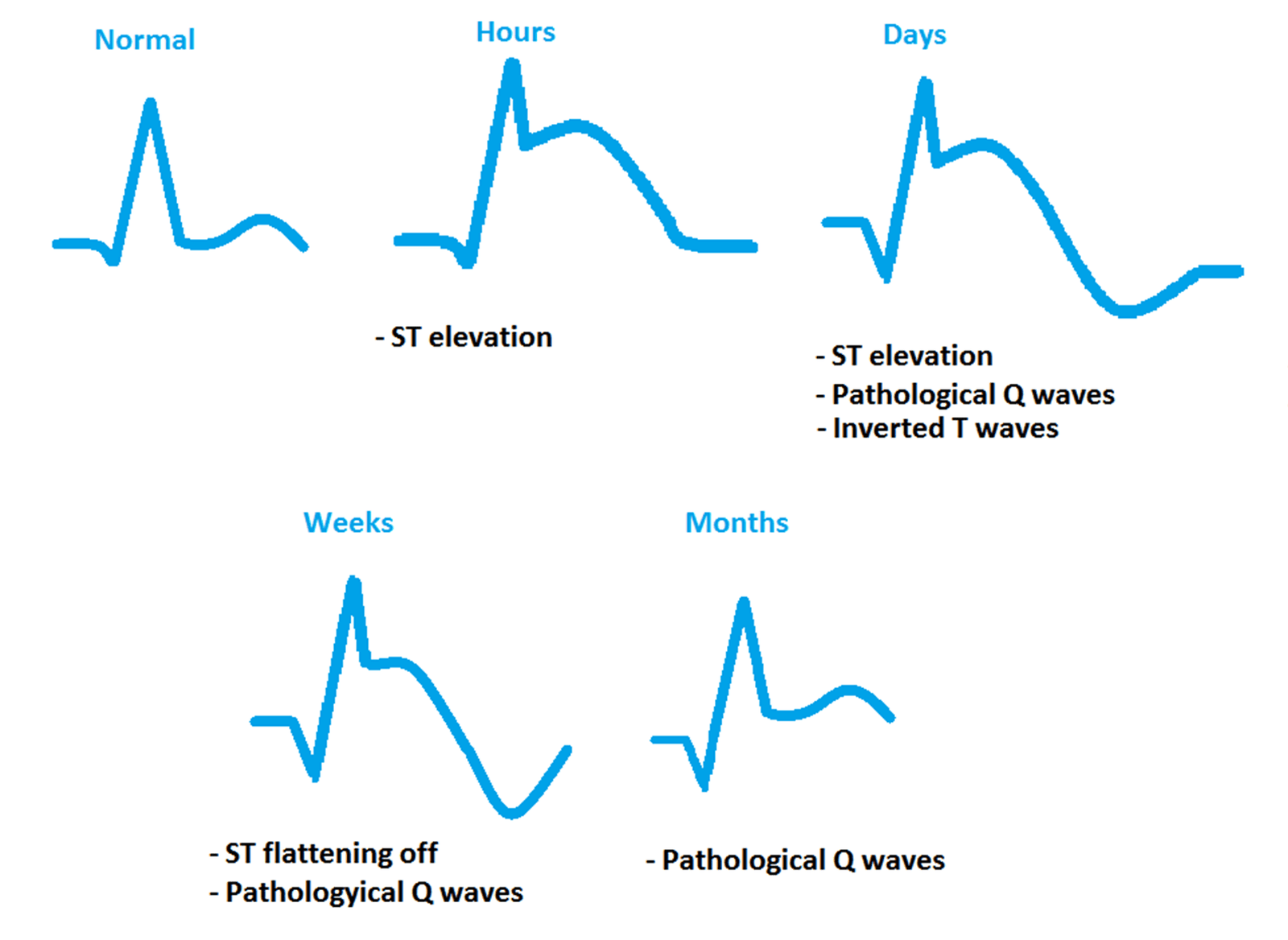
ECG Changes
Early – Within hours
- Peaked T wave (very tall T wave)
- Raised ST-segment
Within 24h
- Inverted T waves – This may or may not persist
- ST segment returns to normal. Raised ST segments may persist if a left ventricular aneurysm develops
Within days
- Pathological Q waves form – Q wave is pathological if it is >25% of the height of the R wave, and/or it is greater than 0.04s width (1 small squares) and/or greater than 2mm height (2 small squares).
- Q waves are also a sign of a previous MI – the changes in Q waves are generally permanent. The changes in T waves may or may not revert. The ST segment can return to normal within hours.
Typical picture of changes
ST elevation – then later, T inversion – , then later, Q wave appears
Other patterns of ECG change
- ST-depression
- Reciprocal change – Sometimes seen in STEMI. This refers to a phenomenon whereby there is ST DEPRESSION in some leads, in the presence of ST elevation in others.

ECG showing Inferior STEMI. Note the marked ST elevation in leads II, III and aVF, and the ST
depression on V2, V3 and V6 (often termed ‘reciprocal change’ when it is associated with ST elevation
in other leads). Also note that there is not (yet) any T wave inversion in this patient.
Troponin Testing
Generally we sue Traditional troponin testing, but the newer high sensitivity troponin is recently very helpful to diagnose. Two types of troponin can be tests for – troponin I and troponin T.
Traditional troponin
- Traditional troponin is a positive or negative test. Serial troponin tests are performed over several hours (typically over 6-8 hours), and any detected troponin results in a “positive” test, and therefore a diagnosis of NSTEMI.
- Troponin levels rise from 2-24 hours after onset of pain, and peak at around 24 – 48 hours, and return to baseline in 5-14 days
High sensitivity troponin
- The recommended test method is TWO troponin tests, 2 hours apart, within 3 hours of the onset of chest pain
- A single negative troponin test is acceptable as a ‘rule out’ (for ACS) if it is >3 hours since the onset of pain
- A positive test is defined as an increase in troponin between the two tests.
Management
Acute Management
- Aspirin 300mg orally – unless an obvious contraindication
- Pain relief, e.g. 5-10mg morphine + metoclopramide (anti-emetic)10mg IV
- Sublingual GTN (unless hypotensive)
- Oxygen – if saturation are <94%
- Troponin kit test and Serial ECGs are a very important part of the emergency work-up of chest pain
Definitive management
STEMI
For STEMI, reperfusion strategy can include fibrinolytic therapy or immediate PCI
- PCI should be considered for all patients presenting within 12 hours of onset of pain. PCI can involve either balloon angioplasty or primary coronary artery stenting
- Primary PCI – PCI given within the 120 minute window
- Rescue PCI – PCI after failure of thrombolysis
- Facilitated PCI – PCI deliberately planned in conjunction with thromboylsis – has no proven benefit over PCI alone
- If angioplasty is not available, give Thrombolytics. The British Heart Foundation advises that it should be given no greater than 90 minutes after initial onset of chest pain, and ideally no greater than 60 minutes if possible. Streptokinase, reteplase or tenecteplase are commonly used thrombolysis drugs
- Give heparin e.g. unfractionated heparin infusion (follow local hospital guidelines), or low molecular weight heparin (e.g. enoxaparin – for 2-8 days)
- Give a glycoprotein IIb/III inhibitor. These are usually given alongside PCI and reduce the risk of immediate vascular occlusion. e.g. abciximab, eptifibatide, and tirofiban
- In conjunction with Aspirin, long term use of Clopidogrel is associated with better outcomes. Prasugrel or Ticagrelor are alternatives to Clopidogrel
NSTEMI
- PCI is also considered first line treatment for those with high risk NSTEMI
- Thrombolysis is NOT INDICATED for NSTEMI
- In conjunction with aspirin, long term use of Clopidogrel is associated with better outcomes. Prasugrel or Ticagrelor are alternatives to Clopidogrel
After Acute Event
- Start a β-blocker – Usually atenolol 5mg IV. Do not give if asthma or right ventricular failure
- ACE-inhibitors
- Statin should start as soon as possible for all ACS patients, regardless of cholesterol levels
- Consider DVT prophylaxis
- Constant ECG monitoring
- Cardiac enzymes ( Every day for 3 days )
Long term management
- Changes in lifestyle: Regular exercise, diet modification, weight loss.
- Smoking cessation
- Reduction in alcohol intake
- COBRA – A mnemonic for Secondary Prevention in ACS
C – Clopidogrel – Antiplatelets
O – Omacar – Omega 3
B – Bisoprolol – β-blocker
R – Ramipril – ACE-i
A – Aspirin
A – Atorvastatin – very potent statin!
Complications
- Dressler Syndrome
- Cardiac Rupture Syndrome
- Cardiac Failure
- Arrythmias
- Cardiac tamponade
- Tachyarrhythmias
- Mural thrombus
- Mitral valve incompetence
- Ventricular aneurysm
Dressler’s syndrome
An autoimmune pericarditis, provoked by MI. Occurs in 5-10% of cases of MI. Onset 1-3 weeks post MI. Localised pericarditis. Causes fever, pericardial effusions, anaemia, raised ESR, enlarged heart on CXR, pericardial rub (on auscultation). may be similar to PE – another post-MI complication. It is often self-limiting, and symptoms last a few days. Treated with NSAID’s, and in more serious cases, steroids.
STEMI vs NSTEMI
#Know more about ischemic heart disease from “THIS LINK”.
#We Partnered with Achievable.me. Check out their website for awesome study content.




very brief and informative. THANK YOU DR. Aastha jain
Thank you very much Dr Jain. As a nursing student in this is very helpful.